Webinar recap: Harnessing the Power of Digital Patient Engagement

A powerhouse panel explores how to optimize patient outcomes by integrating behavioral science, design thinking, and emerging technologies.
The global health industry invests billions in the development of drugs, devices, and therapeutic services to prevent and treat the burden of disease. Yet, if patients don’t follow care plans as advised, the effectiveness of all of those recommendations goes out the window.
Patient disengagement and deferral of care are costly problems for the healthcare sector. A Gallup poll revealed that a record 38% of Americans put off medical care last year. Care deferrers are more likely to rely on urgent or emergency care, experience complications, and accumulate higher costs. The healthcare industry is looking to meet the moment with a more collaborative, connected approach to patient-centered care. And as technology advances, from AI to wearables, the opportunity to leverage digital solutions for improved health outcomes has arrived.
This aspiration, to deliver meaningful innovation for patients by integrating behavioral science, design thinking, and emerging technologies, was the topic of a recent webinar moderated by Jay Erickson, Chief Innovation Officer at Modus. “Harnessing the Power of Digital Patient Engagement” featured special guests the Honorable David J. Shulkin, M.D., Former Ninth Secretary, U.S. Department of Veterans Affairs; Amy Bucher, Ph.D., Chief Behavioral Officer, Lirio; Eric Thrailkill, Chair, Nashville Project Healthcare; and Fred Kopplow, SVP Healthcare Innovation, Modus.
The panel discussed the fundamentals of behavioral science and design thinking, real-world issues and motivations driving patient decisions, and the immense potential for integrated data and precision intervention to build trust, increase equity and access, and make crucial progress on the path toward patient empowerment.
What is behavioral science?
Bucher, a leading expert on applying the psychology of motivation to design, defined behavioral science as both a process and an approach. As a process, behavioral scientists use the scientific method to prove evidence-based hypotheses and measure impact on patient behavior. As an approach, behavioral science is concerned with understanding the factors that make people more or less likely to make choices and take actions related to their health.
“Which can include their cognitions and beliefs, their emotions, their prior experiences, and their mental models,” said Bucher. “There's often cultural factors. Around the world, people practice healthcare differently and consider different behaviors acceptable or not. It has to do with the social and the built environment. Obviously, human beings are complex, and we live in complex contexts that change over time. So if we can sort of take the scientific method and apply it to understanding the reasons why people engage in their healthcare or not, we start to get a sense of the modifiable variables that are in the ecosystem that we can use as levers to get people to engage in their behaviors more frequently or not.”
What is design thinking, and how is it applied in healthcare?
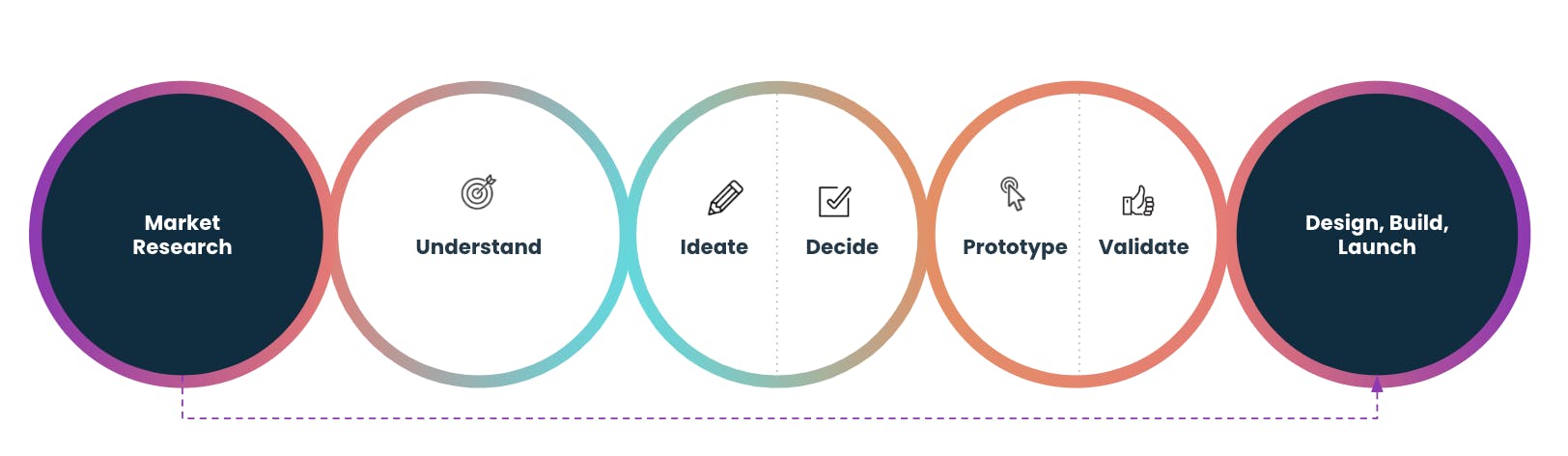
Similar to behavioral science, design thinking is a test-and-learn approach to ensuring that digital products and services meet the needs of users. There are generally five steps in the design thinking approach: Understand the problems facing a set of people, ideate solutions, decide which solution(s) to focus on, prototype, and validate.
As Erickson explained, “Design thinking integrates the needs of people, the possibilities of technology, and the requirements for business success,” he said. “That is so critical, because oftentimes, especially at large organizations, it becomes organization-centric design: ‘What does the organization need?’”
While behavioral science is aimed at the “Big E” of engagement with care or health behaviors — the effect (see our article on the three e’s of patient engagement) — UX designers are focused on the “little e,” or the experience. “You’ve got to get people engaged with our systems in order to get to the Big E,” said Erickson.
On the subject of patient engagement, Erickson asked Secretary Shulkin to highlight some of the issues facing the healthcare industry today.
Understanding the spectrum of patient needs and motivations
Remarkably, as former Secretary, Dr. Shulkin regularly saw patients while representing 21 million American veterans and overseeing the nation’s largest integrated healthcare system with over 1,200 sites of care. “What I typically have always done in my career is I've put on a white coat and a stethoscope and gone in and took care of patients and understood what the experience was like at the ground level,” he said.
Secretary Shulkin shared several examples of a-ha moments at the V.A. He recalled how he would recommend an electronic, mail-order service for refilling prescriptions, but patients often turned down the offer, preferring instead to physically go to their local V.A. pharmacy, even if it meant waiting for a long time. “They would say, ‘That's okay, I'd like to sit there in the lobby with my buddies and talk about what we used to do when we were in the service,’” said Secretary Shulkin. “And so it was that sense of community and that ability to be with their peers. That was really important to them about the V.A. experience.”
I began to understand what this experience was like for veterans, and I did it very much through my own ability to be a caregiver.
Secretary Shulkin also shared a heart-wrenching story of a young patient who initially puzzled him. “I generally take care of more serious chronic problems, and I couldn't figure out why he was in to see me, he didn't have anything really wrong with him,” said Secretary Shulkin. “I finally said, ‘Look, what why are you here?’ And this is in Manhattan in New York City. And he said to me, ‘Because I'm homeless. I've been living in Central Park for four months. I was discharged from the Army. They used to cook all my meals, tell me where to live. Tell me what to do every day. I'm lost. I don't know how to do any of that.’ So, you know, I began to understand what this experience was like for veterans, and I did it very much through my own ability to be a caregiver.”
Bucher agreed that understanding patients’ personal and unique needs and preferences is key to improved engagement. “If you're pushing everybody to go for the mail order prescription, you're essentially disengaging a group of people who feel like they're not being seen,” she said.
Leveraging technology for patient engagement
While the advancement of digital tools such as telehealth platforms have made it easier for providers to communicate with patients, research shows that engagement dwindles quickly without long-term behavior change.
If we push people too hard on something that they've said they don't want to do, we might get them to do it the one time, but we are not going to get that sustained engagement, we're not going to build that relationship that is fueled by mutual respect and trust.
Bucher elaborated on the subject of non-adherence, or when patients choose not to follow their medical instructions, such as refusing to take a medication or not following through with their care plan. “It is so frustrating for clinicians … when you're faced with a patient who says, ‘I don't want to do that’ or ‘I don't like those side effects.’ … But from a behavioral science perspective, we really need to respect that because the evidence is clear that when we force people to take action, we might be able to get them to do a thing once or twice. But healthcare really is about sustained engagement over time, with behaviors that add up to better health outcomes. And if we push people too hard on something that they've said they don't want to do, we might get them to do it the one time, but we are not going to get that sustained engagement, we're not going to build that relationship that is fueled by mutual respect and trust.”
To achieve meaningful behavioral change, the industry will need to find a way to connect siloed data, said Thrailkill, a technology strategy leader who specializes in supporting entrepreneurs and innovators to grow and scale healthcare solutions. “There are a plethora of monitoring devices and wearables that now are able to stream data, large amounts of data that can be analyzed and used for engagement strategies,” he said.
Kopplow, who was formerly the Director of Digital Health for Blue Cross Blue Shield Michigan before joining Modus, is also passionate about connecting the digital dots of healthcare. He said there’s an opportunity for the industry to reimagine digital health with a focus on behavioral science and patient-centric UX. “[We can] correct some things that we couldn't see before,” he said. “We need to nudge more members along. The journeys aren't broken, but I think we have the opportunity to get more people in care to inform and educate.”
The panelists agreed that a personalized approach, perhaps powered by AI and machine learning, will go a long way to building trust by matching messages and interfaces with individual preferences, needs, and capacities.
Learn more
Be sure to watch the full webinar recording for more insights from this expert panel. To keep up with the latest webinar and event invites from Modus, please sign up for our newsletter below.



